How to Reverse Polycystic Ovarian Syndrome (PCOS)
We examine a couple of articles from top journals, and I explain in simple terms how you can reverse your PCOS in weeks or months. Please spread the word as PCOS is becoming more common.
There are many causes of infertility but PCOS is one of the most common
PCOS is the easiest cause of infertility to treat
Most women with PCOS can reach full remission through intermittent fasting and lowering dietary carb intake within a few weeks or months
A high insulin level leading to insulin resistance is the primary cause of PCOS
Although researchers now recognize that PCOS can be successfully treated through diet, it often takes decades for such info to trickle down to medical schools and practitioners
Most people with PCOS have never been told by their doctor that there is a simple, free cure
That’s why you have me 😁
If you have PCOS, spend three months eating very low carb (less than 20 grams of carbs per day) and fasting for at least 16 hours per day.
How To Reverse Insulin Resistance with Diet
First, if you have PCOS, go ahead and just buy Fung’s book The PCOS Plan. (I don’t get any money from promoting it.) I just think that if you really want to cure PCOS, you need a book with a solid plan. Reversing PCOS is going to take some work and commitment. Rethinking how and when you eat is a big deal. Arm yourself with information. Knowing how diet transforms your body will provide motivation. The book explains what PCOS is and why diet works.
Second, get a fasting insulin test done at your doctor or at LabCorp or QuestLab. An ideal fasting insulin score is 2.0-3.0. Anything under 5 is decent. Between 5 and 10 it too high. It’s common for my clients to be 15 or higher at first. I have a few clients with fasting insulin in the high 20s so ten times what it should be.
Another test to consider is called a postprandial (or after meal) insulin test. This would mean getting an insulin draw one hour after eating a high-carb meal. If your insulin spikes unusually high, you are very sensitive to carbs and need to greatly limit them. Some people have a somewhat normal fasting insulin but a very high postprandial insulin response. I encourage people to test this because it’s very encouraging to see it change after working hard on diet changes and fasting.
The chart below shows different postprandial responses to insulin.
A healthy postprandial insulin response one hour after finishing a high-carb meal is about 75 units as shown in the green curve in the graph. (Note: Eating a high-carb meal is done just for the test.)
I get my own insulin tests done by ordering through Marek Diagnostics. You add the fasting insulin test to your cart (it’s $15), pay for it, print out the form, and walk into the LabCorp with the piece of paper. They will not know you used a website instead of a doctor for the order, nor will they care.
Third: Begin Intermittent Fasting.
Start with 16:8 fasting, meaning fast for 16 hours and eat all your food within 8 hours. (Click here for info on how to start fasting).
Most people with PCOS will need to use some advanced fasting strategies. But don’t start these until you’ve eased into fasting by doing at least one month of 16:8. (Here is a post explaining advanced fasting strategies.)
Continue tweaking your fasting window until you have lost any abdominal fat so that the largest part of your stomach, when relaxed, is less than half your height. If you’re 5’ 4” so 64” tall, you’ll know you’ve reversed your insulin resistance when the largest part of your belly (usually just below your belly button, not your natural waist) is down to 32” when relaxed.
Fourth: Greatly reduce carbs.
I recently asked a friend how her daughter with PCOS was doing using diet as a strategy and if she was seeing improvements. She said the diet didn’t seem to be working. Then she told me that her doctor had recommended this PCOS patient have between 100 and 300 grams of carbs per day! Although I was thankful that this doctor acknowledged a PCOS-diet relationship, since few do, I was not surprised that the diet wasn’t working.
Here’s the deal: 100-300 grams of carbs is a lot for the average person who doesn’t have PCOS! For someone with PCOS, it’s way too much. Ideally, someone with PCOS should aim to keep carbs under 20 grams/day until in remission.
Remember, if you have PCOS, you have a disease. Diseases require radical interventions to reverse. Once you no longer have the disease, you’ll likely be able to add back in a few more carbs.
But at the beginning, you need to get in the mindset of war.
Declare total war against PCOS!
Fasting and low carb are your weapons. Sugar and carbs feed the PCOS monster. Do you want to get better? The ball is completely in your court.
God has provided a way for your body to heal but you must put in the hard work.
Doing it kinda ain’t gonna do nuttin’. Do it all the way.
Get out your calendar and mark off three months when you will make total war with PCOS.
Here’s the deal: You get to choose your own adventure. If you work really hard, you will conquer it. If you fool around with sweets every day, sorry, PCOS will continue to wreak havoc in your body.
One thing that’s hard to believe when you’re caught in a sugar and carb addiction cycle is that you really can change your tastes to prefer less carby things. But you’ll never know unless you push through the initial phase.
Why Don’t Doctors Tell You the Cure?
When I first heard Dr. Jason Fung say that PCOS is caused by high insulin and easily cured through diet changes, I felt frustrated on behalf of the many women I know with PCOS who went to doctors and fertility clinics for years and yet never heard insulin or diet mentioned once.
I have one client with PCOS who visited fertility clinics for twenty years and spent tens of thousands of dollars on treatments, and no one ever once mentioned low carb and fasting as a possible treatment.
How could it be a doctor or clinic’s sole job to treat infertility and yet not be familiar with the number one underlying cause of PCOS?
Is this secret information that no one’s ever heard of?
Does anyone outside of Dr. Fung know this?
Inquiring minds want to know.
So I hopped onto Pubmed (as one does) to see if Fung was, in fact, the only person on the planet who knew this hot piece of info.
And low and behold, the words “PCOS and insulin” returned 701 PAGES of results! Now, although I’m an uber-nerd who devours scientific studies as a monkey devours bananas:
(Me reading scientific studies in my room day and night, be like 👆🏻)
In this case, I must confess to not having read through most of those 701 pages of results.
But I did read this first hit, a review of multiple studies. Reviews are always nice because instead of me reading dozens of studies and summarizing them, someone summarized them all for me (this gives me more time to devour other studies).
The study titled Association of Insulin Resistance and Elevated Androgen Levels with Polycystic Ovarian Syndrome (PCOS): A Review of Literature concludes:
The overexposure of androgen is directly linked with insulin resistance and hyperinsulinaemia…However, the overexposure of androgen has direct and specific influence on the development of insulin resistance. Although many factors are involved, resistance to the insulin and enhanced level of androgen are considered the major causes of PCOS. In the present review, we have focused on the pathophysiology and major revolutions of insulin resistance and excessive levels of androgen in females with PCOS.
So there you have it folks. Hit #1 on Pubmed for all the world to read spells it out for the laziest of lazy fertility doctors in the clearest language possible: high insulin (hyperinsulinemia) and the sister problem of insulin resistance lead to overexposure to androgens and then PCOS.
So let me get this straight. You are a fertility doctor. Your entire life is devoted to helping women get pregnant. The most common reason they can’t get pregnant is PCOS. You’ve devoted your whole life to studying PCOS but you somehow missed the major cause. No one’s ever mentioned it to you? You’ve never read a single medical paper on it?
You’ve never once opened up Pubmed and read the top hit on the cause of PCOS?
You had one job. You literally had one job.
Or maybe they do know that PCOS is caused by high insulin but they fell asleep for the 5-minute presentation during medical school where the teacher hurriedly put in a quick bit about how both high insulin and insulin resistance can be cured without drugs with a bit of fasting and low carb eating. Since such things can only be spoken of while the drug rep is not in the room, if at all, it can be easy to miss.
However, the fertility doc could have opened up Google and typed in: “How to cure insulin resistance.”
This is quite an amusing exercise, by the way. The top hit is this article posted on the American Diabetes Association website (or, as Substack writer Nina Teicholz calls it, The American Get-Diabetes Association). This is one of the most underwhelming articles I’ve ever read in my entire life. I could have written a better one in third grade.
Here is one downright exceptional line from it:
Just why a person fails to respond properly to insulin is still a mystery.
Newsflash: I knew more than that about insulin resistance in the first 30 seconds after I began reading about it. I was about two and a half sentences into Jason Fung’s book The Diabetes Code when I knew why a person fails to respond properly to insulin.
But since the ADA only receives $2.6 BILLION (that’s with a B) in funding per year, how could they be expected to know the solution to the single most important problem in all of diabetes? You know what: maybe we need to give them more money.
There’s not a single mention in that ADA article about reducing carbs, or even reducing refined sugar or any mention of fasting. It does say to lose weight and exercise, but do we need an organization with an annual budget of $2.6 billion to tell us that morsel of sage advice?
Then finally, after giving zero helpful advice about what causes insulin resistance and how to combat it, we’re left with this lovely motivational phrase:
Did you catch that? “We don’t know what causes insulin resistance but don’t give up.” Heartening, isn’t it?
“You’re not alone [most of America also has insulin resistance—comfort yourself with such words], lose weight [as if there’s an overweight human on the planet that needs to be told that], exercise more [ditto last comment], and let big daddy pharma sell you some pills, and everything’s gonna be just fine.”
Sorry, I got really distracted by clicking on Google results.
Oh no! Oh no! Google result #3 says:
To self: “Don’t click on it. Don’t do it!” Okay, I’m not going to click on it.
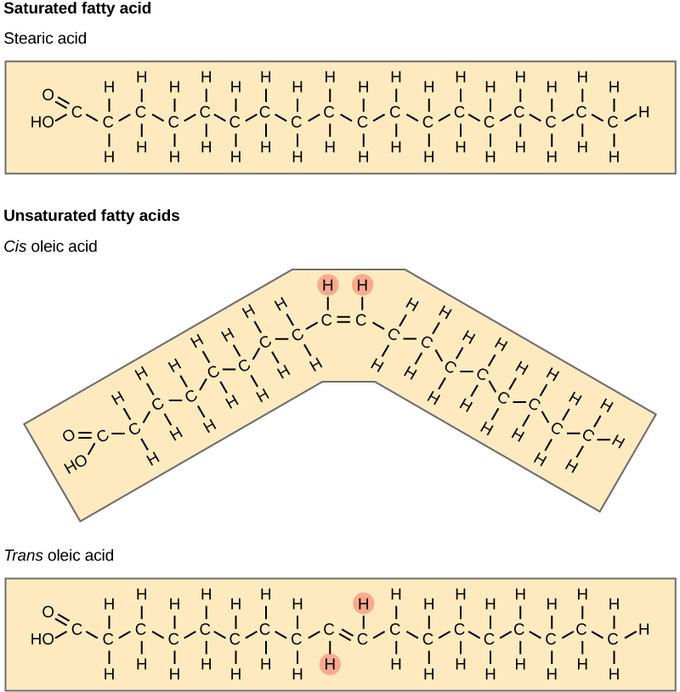
But did I just read: “Swapping out saturated fats for the HEALTHY ONES [veg oils]”??? And “less meat, full-fat dairy, and butter”??? Ummmmm, someone who writes for WebMD needs to go back to 9th-grade chemistry where they showed you a picture of a saturated fat molecule and told how the word “saturated” means “stable” and how the “unsaturated” ones (which WebMD mistakenly calls the “healthy” ones) have multiple kinks in them making them unstable in the body so causing oxidative stress. (More on that in this post: The Skinny on Saturated Fat: It's Vital for Health and Doesn't Cause Heart Disease.)
See kids. See the kink in the UNsaturated fat molecule. The kink makes it UNstable. Now remember that when you grow up. Because every time you read something on a mainstream health website or mainstream news article, it will be a test. They publish the opposite info to see if you’re paying attention. Tricky, isn’t it?
Okay, hold on a second while I write myself a quick note:
Okay, I’m back. Sorry, I got a bit sidetracked.
Okay, so clearly Mr. Clueless Fertility Doc might not be able to learn how to cure insulin resistance by reading the first page of Google results. The state of Google is much worse than I imagined.
But surely some latent knowledge of the human body would cause any fertility doctor with two brain cells to reason: eating a high-carb diet raises insulin, and high insulin causes PCOS. Therefore, eating fewer carbs lowers insulin levels, and lower insulin reduces PCOS. Is this rocket science?
The Pathology of PCOS
In 2017, the journal Diabetes Research and Clinical Practice published a study called Insulin and the Polycystic Ovary Syndrome. The abstract reads:
PCOS [polycystic ovarian syndrome] is characterised by hyperandrogenaemia, hyperinsulinaemia, and deranged adipokines secretion from the adipose tissue. In addition to the reduced insulin sensitivity, PCOS women exhibit β-cell dysfunction as well.
Let’s break this down to language that the average person can understand. Hyperandrogenaemia simply means that a person with PCOS has too many androgens, hormones typically thought of as male hormones such as testosterone. All females need some testosterone but in women with PCOS, their body is making more than the average female. The excessive androgens lead to not only cysts but also possibly facial hair, male pattern hair thinning, and acne.
The overproduction of androgens is related to the next big word in the above quote: hyperinsulinemia, or high insulin levels. Insulin is a master hormone with over 200 jobs in the body (most hormones have only two or three). When insulin is chronically elevated in response to high carb intake, over 200 different kinds of cells are affected.
Remember that insulin stimulates the growth of fat tissue. When insulin is low, the body can tap into stored fuel in the form of body fat. But when insulin is high, the body is signaled to store fuel and grow fatter (think bear in the fall).
In the case of PCOS, high insulin levels overstimulate the ovaries to form cysts which grow out of control. This is because insulin is a growth hormone. Just as it causes your thighs to grow, it also causes the cysts in your ovaries to grow.
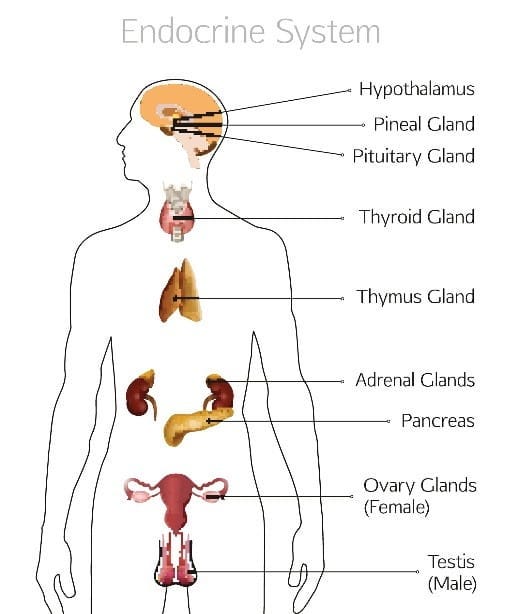
By way of review, here’s a picture of the endocrine system:
The endocrine system is involved with:
Metabolism
Homeostasis (constant internal balance), such as blood pressure and blood sugar regulation, fluid (water) and electrolyte balance and body temperature
Growth and development
Sexual function
Reproduction
Sleep-wake cycle
Mood
Here’s something to notice about the seven main functions of the endocrine system listed above: reproduction and nutrient metabolism are intimately connected since they’re both a part of the endocrine system.
The science seems quite straightforward to me. If there’s a dysregulation in metabolism, there may be a problem in the other parts of the endocrine system since they’re so closely integrated.
Finally, let’s tackle the last two tough bits from the quote above. First, the study said that people with PCOS have:
deranged adipokines secretion from the adipose tissue.
Adipokines are a type of cytokine. This is a molecule that is released from a cell in distress that signals to other cells something is wrong. This signal causes the body to be in a constant low level of inflammation.
The phrase “adipose tissue” simply refers to fat tissue. The article tells us that one of the characteristics of PCOS is having fat tissue that is sending out inflammatory signals to the rest of the body. We all have a personal fat threshold or an amount of weight over which our cells are unhappy. For some people, this threshold is very low. The fat cells get filled beyond their comfort zone and this sends inflammatory signals to the body. This can negatively affect fertility because the adipokines are signally to the body that you are too unhealthy to carry a baby.
Beta Cell Dysfunction
The study quoted above said:
In addition to the reduced insulin sensitivity, PCOS women exhibit β-cell dysfunction as well.
β-cell dysfunction (pronounced beta-cell) refers to the cells in the pancreas that are responsible for making insulin. When a person’s insulin is either chronically elevated, or spiking very high after each meal, the β-cells can eventually become exhausted and stop working correctly. β-cell dysfunction eventually leads to high blood glucose levels as the pancreas becomes burned out.
It can also lead to type 1 diabetes which happens when the immune system attacks and kills the β-cells in the pancreas. (My current working explanation of autoimmune disease is the body attacks tissue because it is damaged, not that the tissue is damaged because the body mysteriously attacked it. Of course, the immune attack causes further damage.)
It’s a funny world that we live in. The choices that we make about how we eat have consequences. Not everyone can be healthy and eat whatever they feel like and have no negative consequences. Our bodies are sensitive to food and the systems are interconnected. Bodies can handle some abuse but they can also get overloaded.
For most people suffering, it’s not that they they’re gorging themselves because they don’t care so. It’s that they’ve never been told that PCOS has a simple cure. It’s amazing what information can do.
Results
You should notice lighter periods, acne clearing up, less facial hair, and cysts should stop forming when you’ve successfully cured your insulin resistance or PCOS. You may need to eat somewhat lower-carb and fast for life. But this becomes extremely easy once you get in the groove—much easier than living with PCOS.
As with anything in life, results will vary. An acquaintance of mine was unable to get pregnant for 8 years due to PCOS and got pregnant the same month that she began intermittent fasting. But that result is extremely unusual. For most women, it will take several months.
Be sure to watch this video with Dr. Nadia Pateguana where she tells stories from her years of clinical experience helping women with PCOS get pregnant using fasting and a low-carb diet. Funny story: she stumbled on the cure by accident. She was originally running a clinic to help women with metabolic health, and they surprisingly kept getting pregnant after years of infertility even though they came merely wanting to lose weight. Along the way, she realized that she had PCOS herself.
One important point she makes in the video is that PCOS can occur in patients who have a normal BMI even though one is much more likely to get PCOS if overweight. One mistake I’ve seen doctors make over and over is to think in black-and-white terms. I have a friend who showed many signs of PCOS but was told by several doctors that she couldn’t possibly have it since she wasn’t technically considered overweight. This rigid thinking fails to budget for the complexities of the human body.
It’s possible to have high insulin levels without being overweight. The body fat percentage is much more important than the weight on the scale, particularly if one has hidden abdominal fat. Some people are extremely sensitive to carrying extra fat around the middle and will develop PCOS when they have even a small amount of hidden abdominal fat.
This was the case with Dr. Pateguana. Even though she was not technically overweight, she was sensitive to carbs. She carried just enough fat around her middle to give her PCOS. When she changed the way she ate, her PCOS disappeared.
Here are some additional other things to consider if struggling with infertility.
Iodine Supplementation: one doctor who’s studied this extensively is Dr. David Brownstein. You can order his book here or listen to him explain the key concepts from his book in this video. He has over 20 years of experience watching patients benefit from iodine supplementation.
Estrogen Dominance: this is interconnected with high insulin and low thyroid function so fasting may correct estrogen dominance. Often iodine supplementation can enhance thyroid function leading estrogen dominance to heal. In some cases, progesterone supplementation may help fertility and offset estrogen dominance. You’d need to see a functional medicine practitioner who can prescribe bioidentical progesterone. You can also tackle estrogen dominance by eating large amounts of cruciferous vegetables such as broccoli, cauliflower, kale, and brussels sprouts. A chemical in those veggies called sulforaphane binds to the estrogen in the gut.
Stevia: read my post on stevia and how it may negatively affect fertility.
Read to get serious about fasting? Don’t miss my Fasting Course: Finding Success Intermittent Fasting.